Restless Leg Syndrome (RLS) is a common affliction which affects as much as 10% of our population, particularly those middle-aged or older. Women are also more prone to RLS, although it can be found amongst men and younger people as well.
Often caused by a combination of mental and physical factors, RLS can be treated at home and without a doctor’s care, and with treatment typically involving some monitoring and a few simple lifestyle changes.
However, if you do suffer from it, not only can it be uncomfortable—particularly while in confined spaces—it can also lead to difficulty falling asleep and staying asleep.
Here is what you need to know about RLS, its effects on us, and how you can best mitigate its effects.
What is Restless Leg Syndrome?
Restless Leg Syndrome is can best be described as an unpleasant twitching, cramping, or tickling sensation in the leg muscles which urges the sufferer to move to seek relief.
So far as causes for these symptoms, there are both mental and physical explanations for why they occur, which we will go over after helping you understand just what RLS is.
First, there are 2-types of RLS: Primary (AKA Idiopathic), and Secondary. There is also a similar disorder which can lead to RLS called Periodic Limb Movement Disorder (PLMD) in which limbs (most often legs) twitch or spasm uncontrollably during sleep. However, for now, let’s consider the 2-types of RLS:
- Primary, or Idiopathic RLS—This is the most common type of RLS, although it is without a known cause, other than that it is likely inherited. It usually starts in childhood and is lifelong, with symptoms typically worsening with age.
- Secondary RLS—With secondary RLS, onset is sudden, and usually due to a disease, medication, or other condition. It usually starts in the mid-forties, and symptoms don’t worsen with age. Symptoms are, however, usually more severe, and can be caused by arthritis, pregnancy, diabetes, kidney disease, iron deficiency, certain medications, or other causes.
It should also be noted that while RLMD is different than RLS, symptoms of it occur in around 80% of patients with RLS. Both also affect sleep by making it hard to fall asleep, and hard to remain asleep due to recurring episodes throughout the night. It is for these reasons that both are classified as sleep disorders which can lead to other problems due to lack of sleep, such as:
- Daytime sleepiness
- Irritability
- Mood swings
- Difficulty concentrating
- Depression
- Depleted immune system
- Weight gain
- Accident proneness
- High blood pressure
While symptoms of idiopathic RLS often get worse with age, some sufferers may go long periods of time without symptoms. However, some symptoms of secondary RLS may be temporary, such as with pregnancy, passing conditions, illness, or medications.
What Causes Restless Leg Syndrome?
First, we need to point out that the word “idiopathic” literally means “…any disease with an unknown cause of apparently spontaneous origin,” per Wikipedia. Clearly, this indicates that for primary RLS sufferers, there is no known source of their condition.
That said, it should also be noted that in nearly half of all primary RLS cases, there is a family history of the affliction, which indicates that genetics may be a primary cause.
However, for those suffering from secondary RLS, there is usually a cause and effect which can be identified. These causes can include:
- Consumption of alcohol—Even though a few drinks may help you fall asleep, alcohol interrupts the deep, slow-wave delta sleep patterns you need for full, rejuvenating sleep. Not only that, it also has been purported to block the production of certain sleep chemicals in the brain which are responsible for maintaining circadian cycles, which leads to sleep interruptions throughout the night, and it can worsen breathing difficulties, such as with sleep apnea.
And, these factors are likely why alcohol often triggers RLS in sufferers, which makes avoiding alcohol before bed a good idea for RLS sufferers.
- Certain medications—Medications such as sedating antihistamines and anti-nausea drugs can inhibit production of your brain’s dopamine, which in turn can lead to RLS. Other medications such as antidepressants and antipsychotic medications can cause an increase in your body’s serotonin production, which can also lead to RLS episodes in the night.
Fortunately, your doctor can usually adjust your dosage to a level where your RLS is more manageable, and in a worst-case scenario, many medications are either temporary, or have an alternative for sensitive users.
- Pregnancy—Often attributed to a lack of iron, around 20% of all pregnant women experience RLS around the 3rd trimester. Your doctor can identify an iron deficiency through a simple blood test, and iron supplements or iron-rich foods are an easy addition to your diet.
Symptoms of RLS will also usually disappear with the end of pregnancy.
- Chronic disease—Diabetes, Parkinson’s Disease, and kidney failure can also cause RLS. However, symptoms of RLS can often be resolved by treating the disease or medical condition.
- Tobacco use—Amongst the MANY reasons to stop smoking or chewing tobacco is its connection with RLS. Not only are tobacco users damaging nearly every other aspect of their health through their habit, nicotine is a stimulant which disrupts sleep in much the same way as having coffee before bed can. This in turn can lead to RLS—not to mention breathing problems, bad breath, high blood pressure, cancer, and…well, you get the idea. Just stop already, okay?
- Caffeine—While most of us understand that caffeine is a stimulant, we may not always know where it is lurking. And, as with other sleep-disrupting substances, caffeine consumption too late in the day, or from an unexpected source can lead to poor sleep and symptoms of RLS.
Remember that foods containing chocolate, some teas (even some “herbal” teas!), and many soft drinks can contain enough caffeine to keep you awake, and your legs restless during the night.
- Stress—It may be your job, your situation, or any one of many other factors which is causing it, but the bottom line is, stress can lead to symptoms of RLS, along with poor sleep.
This is due to stress causing your adrenal glands to release cortisol—AKA, the stress hormone–which it does as a “fight or flight” response. This in turn helps you become mobilized and ready for action, or in other words, the opposite of what you need for a good night’s sleep!
While there are other possible causes of secondary RLS, these are some of the most prominent ones. As you can see, most are related to sleep disruption, meaning if you are suffering from RLS and cannot pinpoint the cause, look for reasons pertaining to your not sleeping well. These can be anything from a magnesium deficiency, to poor sleep hygiene in the sleep chamber.
Mitigating the Effects of RLS
Now that you have some understanding of RLS and its causes, it is time to go over how to manage your symptoms. Naturally, this means first determining the cause of your symptoms, as well as monitoring their effects.
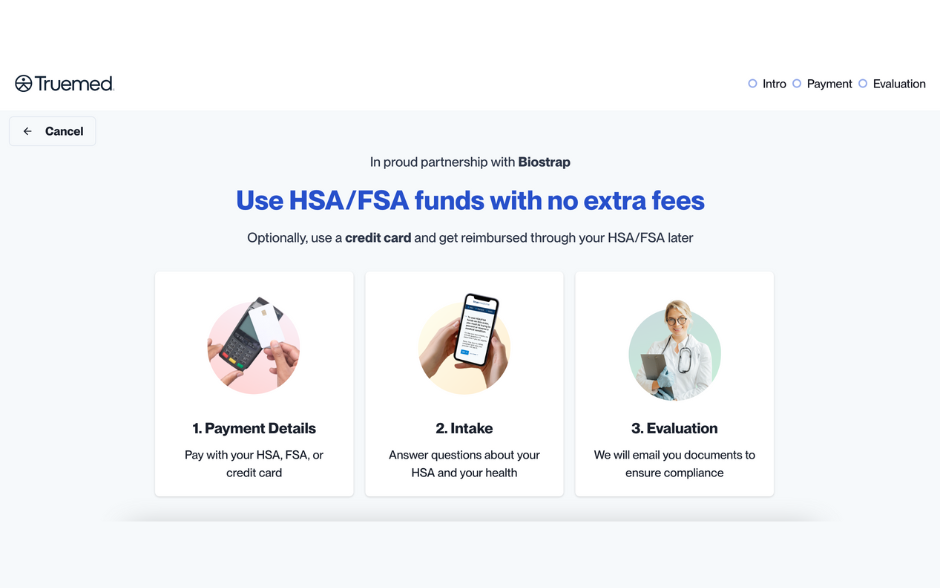
For this, a device such as a Biostrap can be invaluable, since using one can help you track such numbers as Heart Rate Variability (HRV) and Peripheral Capillary Oxygen Saturation (SpO2), both of which are key biomarkers in helping measure the quality of your sleep.
But why is this?
Simple. These biomarkers will help you to understand your sleep habits, as well as to show you the overall quality of sleep you are getting. From this, you can better measure improvements as you go along, as well as to show you what is—and is not—working in your treatments of RLS.
However, let’s start by going over some treatments for your primary and secondary RLS symptoms.
First, sleep hygiene is of key importance in getting a healthy night’s sleep, which in turn can help relieve your symptoms.
But just what is “sleep hygiene” anyway?
Simply put, good sleep hygiene is habits and practices which help to improve the quality of your sleep. These can include:
- Getting some exercise—Daily exercise can help you fall asleep more easily and can also help you stay asleep through the night.
However, you should avoid vigorous exercise, especially within 3-hours of bedtime, since heavy exercise can have the opposite effect of light, aerobic exercise on your sleep. This is because when you do heavy weight training, high intensity interval training, or other forms of anaerobic exercise, your body is producing such stimulating hormones as norephedrine and cortisol, as well as adrenaline, which can remain in effect and keep you energized for hours after your workout.
Instead, try for 15-45 minutes of light to moderate intensity exercise each day, during which you can speak in full sentences without having to pause for breath. This can include walking, light running, swimming, or simply doing things like taking the stairs rather than the elevator during your day.
- Keeping a consistent sleep/wake schedule—Establishing a consistent bedtime and adhering to it is an essential part of good sleep hygiene. This means not only putting down the remote and hitting the hay at the same time every night during the week, but on weekends and holidays as well (sorry!).
By going to bed and waking at the same time each night and morning, you can become a better and more efficient sleeper, which will lead to more sleep overall and a reduction in RLS symptoms.
- Keeping your bedroom quiet, dark and cool—Sleep environment is crucial for good sleep, and by keeping your bedroom dark, quiet and cool, you can help ensure that you are getting the best quality sleep you can.
Try to keep your bedroom at between 60-67-degrees Fahrenheit, and block out any light from outside the room, as well as avoid keeping any lights—even a small night light—off while you are sleeping.
If you live in a noisy, urban environment or have other outside noises which cannot be avoided, try earplugs, or sound-blocking headphones which can also provide soothing sounds or white noise.
- Avoiding blue light screens and all electronic devices before bed—We live in an age where we are constantly either checking our phones, on our computers, or are being entertained by movies and television shows. However, electronic devices and their screens may be the root of your insomnia, since the blue light emitted from electronic screens can stop your body’s production of the sleep hormone melatonin.
Try turning off all electronic devices a few hours before bed, and never watch TV while in bed!
By doing this, you can not only allow your body’s production of melatonin to be on schedule to help you get a fit night’s sleep, you also won’t be tempted to stay up and watch just one more episode of “Law and Order” before finally nodding off.
- Avoiding naps during the day—While a nice afternoon nap may be a tempting way for you to hit your “refresh” button, it is not a good way to ensure a full amount of quality sleep each night.
This is because napping during the day can prevent you from being tired enough to easily fall asleep at night, which can then shorten the amount of REM (Rapid Eye Movement) and NREM (Non Rapid Eye Movement) cycles necessary in good, productive sleep.
Plus, if you are doing a good job of adhering to your sleep schedule, you should be getting enough sleep that a nap isn’t as tempting!
- Sleeping on a comfortable mattress, and with comfortable bedding—What you sleep on can make all the difference in how well you sleep, and it all starts with your mattress. Make sure it is the correct firmness for you, and you should never sleep on one which is too old or worn-out. The firmness rating should match your weight and sleeping type (i.e. side sleeper, back sleeper, etc.), and you should be able to rise after a full night’s sleep without aches or pains—or any groggy, unrested feeling.
Your pillow should also be firm and supportive, and preferably made from natural materials which breath well and remain cool. The stuffing should not bunch up and flatten, and if your pillow is worn out or flat, it is time to replace it without hesitation.
Your bedding should include enough blankets to keep you warm without overheating you, and all bedding should be free of dust and dander, which can hinder sleep with allergies and breathing problems.
Sorry Fido and Fluffy, no more sleeping on the bed!
And, you may also be able to ease the symptoms of your idiopathic RLS with massage, warm baths, and either hot or cold packs, depending on what works best for you.
Other remedies which your doctor can help you with are:
- Iron supplementation or adding additional iron-rich foods to your diet.
- Dopamine agonist to improve dopamine production.
- Dopaminergic agents to improve dopamine production.
- Benzodiazepines, which are sedative medications such as Xanax or Klonopin.
- Painkillers, such as aspirin or Ibuprofen.
Tracking Your Progress
Now that you have an idea of how to improve your symptoms, you can start tracking your results and verifying that things are working, which will show up on your sleep tracker numbers.
For instance, using Biostrap’s Sleep Score as an example, you can measure the quality of your sleep sessions over a 3 to 30-day period, over which such factors as deep sleep percentage, total awake time, time taken to fall asleep, HRV, and SP02 are measured.
Since each of these measures begins with a value of 20 that is reduced whenever it is off, your overall average will show you how much or little your RLS is affecting your sleep.
For example, let’s say that for most of the month, your HRV is doing fine at 20, but you then have a few nights where it drops to, say, 17. Clearly, this means that on those nights, your heart rate was showing more activity in your sleep, which means you likely experienced less deep, delta, or “slow-wave” sleep.
Now, you can also look at other factors which may have influenced your sleep that night. Did you stay up too late worrying about a work problem? Was the weather warmer, which made sleeping more difficult those nights?
Whatever the reason, having these numbers available makes it easy to figure out just what it is, and to avoid repeating it in the future.
Finally
Nothing can ruin a good night’s sleep like an episode of RLS, and nothing can cause your RLS symptoms to flair-up like not sleeping well can.
However, this 2-headed monster can be tamed, although it takes some discipline and understanding on your part of the cause and effect of your symptoms.
By tracking your sleep score and using it to measure a few key biomarkers, you can better ensure that measures you are taking to improve your sleep are reducing the incidents of your RLS. This in turn will lead to a better quality of sleep, as well as better overall health and wellbeing.