Too much salt is bad for you. Everyone knows this. Lose the salt shaker, we’ve been told, by our doctors. Our mothers. The government. Our trainers. Turns out, maybe we should take this advice with, er, a grain of salt. That is, with skepticism.
In a new book The Salt Fix author James DiNicolantonio comes out swinging. Subtitled Why the Experts Got It All Wrong—and How Eating More Might Save Your Life, the book lays out the case that medicine has been ignoring its own research. Study after study, he says, shows the dangers of salt consumption are exaggerated, the risks of a low salt diet understated, and, when it comes to government recommendations? The numbers are just plain wrong.
What is Salt?
Salt (NaCl or sodium chloride) is a mineral made up of equal parts sodium and chloride. Most commercial salt is harvested through mining or solution mining existing salt deposits. Salt occurs naturally throughout the world and is necessary for all life.
Do a quick Google search on ‘tips for heart health”. Nearly every search result will tell you to reduce or eliminate the salt in your diet. Authorities firmly on the no-such-thing-as-good-salt bandwagon include Harvard the British National Health Service, the CDC Centers for Disease Controls and Prevention (CDC), Health.gov and the American Heart Association. The CDC has launched a Sodium Reduction Initiative.
And for people with existing high blood pressure, salt is a serious irritant. Salt reduces their kidneys’ ability to remove water. This extra fluid strains blood vessels and can elevate blood pressure further.
What’s the deal with blood pressure?
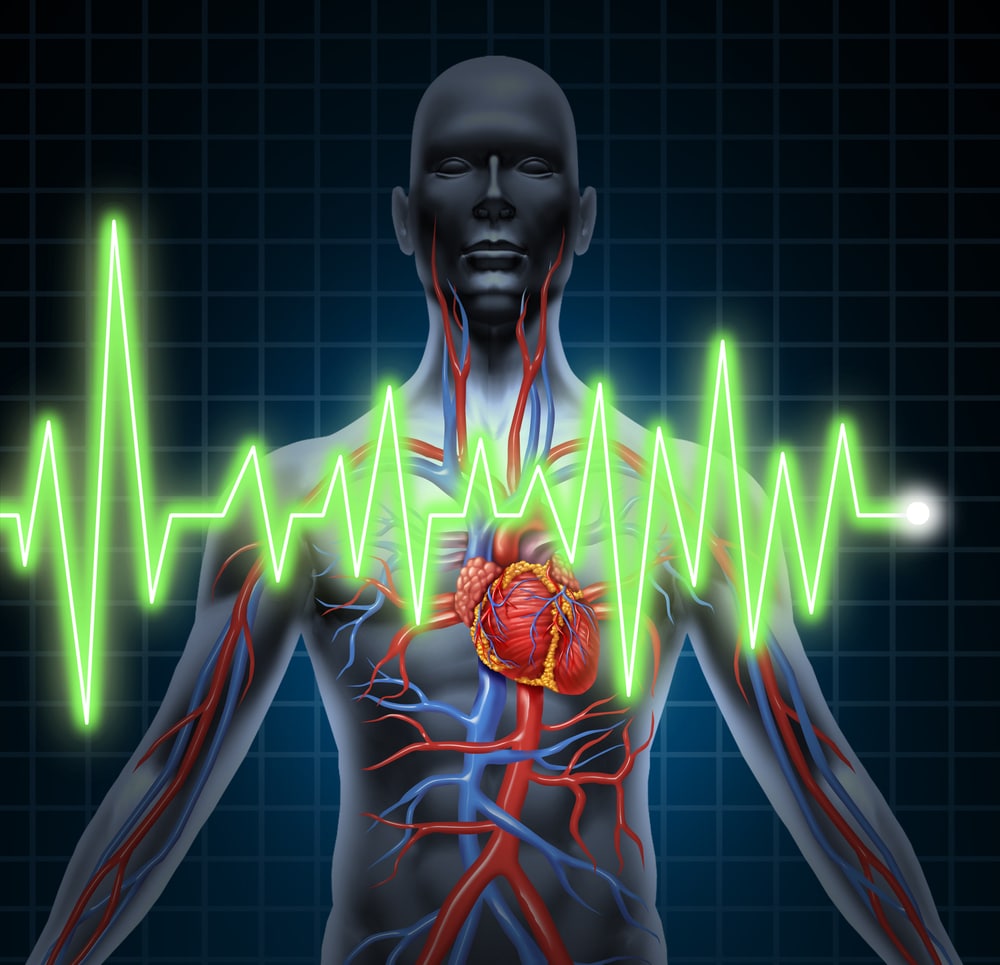
Blood pressure is the measurement of blood moving through the circulatory system. It is measured by two numbers: systolic (the top number, is the pressure in your blood vessels while your heart beats) and diastolic (the bottom number, is the pressure as your heart rests between beats). A normal range is systolic under 120 mmHg and diastolic reading under 80 mmHg. (120/80.) Hypertension (high blood pressure) is diagnosed when systolic exceeds 140 mmHg. Or diastolic tops 90 mmHg.
High blood pressure increases the long-term heart risk and stroke. Dangerously high blood pressure raises the immediate risk of stroke, heart attack, organ failure or death. Low blood pressure can also signify a problem. Plummeting blood pressure from any cause is a life-threatening emergency.
Blood pressure is affected by the heartbeat and the width and elasticity of our arteries. Salt and potassium also work together to regulate blood pressure and circulating blood volume.
Without salt, our bodies could not sustain blood volume. Our blood vessels would literally collapse, leading to circulatory collapse, hypovolemic shock and eventually death.
How Much Salt is Too Much?
Nutrition and health are closely related. Given the demonstrated connection between high blood pressure and poor cardiac outcomes, health officials have sought behavioral interventions to lower blood pressure. Salt, known to raise blood pressure in people with already high blood pressure, was an obvious target. Salt began to be seen as bad in general. The 2015-2020 Dietary Guidelines for Americans recommend less than 2.3 grams of sodium per day. The average American now eats 3.4 grams.
Some people are salt sensitive. High salt intake raises their blood pressure. A low salt diet decreases their blood pressure. Other folks are salt resistant. It’s not clear why. There is no unified theory of what causes high blood pressure. We do know that there is a connection between blood pressure and the ability to maintain core body temperature.
But for people who aren’t salt sensitive, restricting salt intake may not make sense. DiNicolantonio, author of The Salt Fix, says our relationship with salt is ancient as we “evolved from the briny sea”. He posits that healthy adults should actually be consuming 3 to 6 grams, more than double the current recommended limit.
Salt plays a key role in blood volume, hydration, electrolyte balance and general homeostasis.
Salt and our resting heart rate
When exercising, a healthy heart can even double its heart rate and still not cause an unhealthy rise in blood pressure. Blood vessels just get larger (dilate) to allow increased flow. But what about our resting heart rate?
Resting heart rate is a key measure of our overall health. The lower the better. DiNicolantonio is a cardiovascular research scientist and doctor of pharmacy, We reached out to him to ask about the impact of salt on our resting heart rates. “Low-salt diets have been found to increase heart rate in humans in several studies,” he said.
What about heart rate variability?
Heart rate variability (HRV) is the diversity of spacing between each heartbeat. High HRV is a marker of cardiac health. People with high blood pressure have decreased HRV. So what is the role of salt intake in HRV?
Sodium balance and related changes in plasma volume help determine our HRV. High salt diets might affect people with high blood pressure differently, including their HRV. “The data on heart rate variability are less consistent,” says DiNicolantonio, “but it is possible that by chronically stimulating the sympathetic nervous system low-salt diets may lead to altered heart rate variability.”
One study of heart rate variability centered on salt sensitivity and blood pressure. Researchers found that the body makes adjustments to regulate blood pressure. When salt intake is low, the heart and peripheral vasculature increase cardiac activity and vascular tone. When salt intake is high, the body decreases cardiac activity.
New areas of study
In 2014 The National Heart, Lung, and Blood Institute (NHLBI) convened to examine Salt’s Effect on Human Health. This working group “identified scientific gaps and challenges and highlighted some opportunities for scientific inquiry and technical development” concluding, “the initial research that implicated salt as a factor in important diseases points to the need to further illuminate the biological mechanisms and pathological processes to which salt may contribute”.
Specific areas for further study include the role of hypertension in autoimmune diseases; salt-sensitive hypertension; how we store salt in our skin; how to determine salt sensitivity at an individual level; new technologies to measure sodium concentrations in human tissue; and even a Sodium MRI to help reveal the role of salt in health and disease.
DiNicolantonio links low-sodium diets to medical risks including obesity, heart failure, and kidney disease, concluding “overconsumption of salt is not the primary cause of hypertension”.
“Salt restriction. “ he says, “may actually worsen overall cardiovascular health. and may lead to other unintended consequences (insulin resistance, type 2 diabetes, and obesity).”
He just performed an overview of existing research entitled, Is Salt a Culprit or an Innocent Bystander in Hypertension? A Hypothesis Challenging the Ancient Paradigm The study highlights a substantial body of peer-reviewed evidence, and concludes that high salt consumption is not always bad, and low salt diets are not always a panacea. Salt intake is a proven risk for folk who already have high blood pressure. The rest of us could be eating salt (within reason). A low salt diet, says DiNicolantonio, is even potentially heart harmful.
So who’s right? Looks like the debate will continue for a little while longer. In the meantime, know your risk factors, check your blood pressure, monitor your heart rate, get plenty of exercise, and don’t go overboard on the salt. But you might not need to skimp on it either.