Understanding Heart Rate Variability (HRV)
There are a number of metrics we can use to get a snapshot of our health and well-being. From blood pressure to heart rate, doctors and researchers are more interested in our physiological data than ever before, especially heart rate variability in healthy individuals.
There is one marker for resilience and well-being that researchers have just begun to utilize over the past two decades. It’s called Heart Rate Variability, or HRV. This metric, once measured primarily in athletes and those with abnormal heart rhythms, has since become a key piece of data for individuals wanting insight into the state of their physiology and nervous system.
HRV provides profound insights into the autonomic nervous system’s regulation and overall physiological resilience. This comprehensive guide delves into the multifaceted nature of HRV, exploring its significance as a biomarker for health, fitness, and stress management. With advancements in wearable technology and data analytics, HRV has transitioned from a niche research interest to a mainstream tool for individuals and healthcare professionals alike. By examining the factors influencing HRV, such as age, lifestyle, and environmental stressors, this guide aims to equip readers with the knowledge to interpret HRV data effectively. Furthermore, it highlights the potential applications of HRV in optimizing athletic performance, enhancing mental well-being, and monitoring chronic health conditions. As we navigate the complexities of modern life, understanding HRV offers a window into the body’s adaptive capacity, empowering individuals to make informed decisions for improved health outcomes. Let’s dive in!
What is Heart Rate Variability and Why is it Important?
Heart Rate Variability (HRV) measures the variation in time between consecutive heartbeats and reflects how well the autonomic nervous system (ANS) regulates the body. The ANS consists of two branches:
- Sympathetic Nervous System (SNS): The “fight or flight” system that increases heart rate in response to stress.
- Parasympathetic Nervous System (PNS): The “rest and digest” system that slows the heart rate to promote recovery.
HRV reflects the balance between these systems. A higher HRV indicates better adaptability and a healthy response to stress, while lower HRV can signal fatigue or imbalance.
Unlike a metronome, which beats at perfectly regular intervals, a healthy heart varies its time between beats. This variation, known as the inter-beat interval (IBI), shows the heart’s flexibility in responding to different demands. A metronome-like heart rhythm (with no variability) could indicate stress or impaired health, whereas HRV reflects a heart that adapts dynamically to changing conditions.
Heart Rate Variability (HRV) is a measure of the variation in time (in milliseconds) between consecutive heart beats, known as the heart period. It is an important indicator of the autonomic nervous system’s regulation of the heart and is used in the analysis of heart rate and blood pressure. A high HRV is generally associated with a healthy heart and indicates a robust autonomic response, whereas a lower heart rate variability can be a sign of stress or potential health issues, such as congestive heart failure.

What Is a Normal Heart Rate Variability (HRV)?
HRV has a large individual component that has yet to be understood clinically, and therefore is more often used to assess changes in health over time. HRV can fluctuate day-to-day based on exposure to stress, sleep quality, diet, exercise, and more. This leads to low repeatability, and therefore makes normative data difficult to collect.
The table below indicates age ranges and genders and their corresponding average HRV (RMSSD) ranges. Note that these are general guidelines and individual HRV can vary significantly based on factors like fitness level, stress, and overall health.
| 20-29 |
50-100 |
55-105 |
| 30-39 |
45-95 |
45-95 |
| 40-49 |
40-85 |
40-85 |
| 50-59 |
35-75 |
35-75 |
| 60-69 |
30-65 |
25-60 |
| 70+ |
25-60 |
25-65 |
| Age Range |
Men (RMSSD) |
Women (RMSSD) |
Key points
- HRV generally decreases with age for both men and women
- Men tend to have slightly higher HRV than women, especially in younger age groups.
- The difference in HRV between genders becomes less pronounced in older age group.
- The most common HRV for men is around 40 ms, while for women it’s around 37 ms.
- A normal HRV for adults can range from below 20 to over 200 milliseconds, emphasizing the high degree of individual variation.
Long-term vs Short-term Trends
HRV can be difficult to interpret from a single reading because it is influenced by many factors and fluctuates throughout the day. However, tracking both short-term and long-term HRV trends provides valuable insights into your health and well-being.
Short-term Trends:
In the short term, HRV can fluctuate due to immediate factors like stress, sleep quality, hydration, or even meals. A daily spot check might show variability based on these conditions, but such short-term changes can help identify immediate stressors or signs of recovery. For example, a temporary dip in HRV after a hard workout or poor night’s sleep is normal, as the body is dealing with physical stress. However, frequent day-to-day fluctuations can indicate poor recovery or chronic stress, especially if there’s a high coefficient of variation (CV%).
Long-term Trends:
Long-term trends, on the other hand, provide a more stable and meaningful picture. Tracking HRV over weeks or months allows for non-invasive insight into overall health and the effectiveness of lifestyle changes. In general, higher HRV over time indicates better stress management and physiological adaptability. Positive lifestyle habits like regular exercise, meditation, and good sleep hygiene should lead to a gradual increase in HRV. Conversely, a downward trend in heart rate variability may signal issues like overtraining, poor sleep, illness, or excessive stress.
While an increase in HRV itself won’t directly improve health, it reflects healthier adaptations in the body’s ability to handle stress over time.
Understanding HRV and its Role in Health
Understanding heart rate variability (HRV) and its role in health is crucial for both clinicians and patients. Heart rate variability is associated with the autonomic nervous system’s regulation of the heart, reflecting how efficiently the heart is beating. A high heart rate variability is generally indicative of good cardiovascular health, while a reduced HRV may signal underlying health issues. The relationship between heart rate variability and overall health is complex, as various factors can affect your heart rate variability, including stress, sleep, and physical activity.
In clinical settings, heart rate variability analysis is often used to assess the health status of patients with heart failure and other cardiac conditions. Studies have found that HRV can be a predictive marker for adverse outcomes in patients with heart conditions. The analysis of heart rate variability involves measuring changes in heart rate over time, often using heart rate monitors. These devices can track low frequency and other components of HRV to provide insights into a person’s health.
To improve your HRV, practices such as heart rate variability biofeedback and lifestyle modifications can be beneficial. Establishing a baseline HRV and monitoring average HRV can help individuals understand their normal HRV levels and make informed decisions about their health. By maintaining a healthy lifestyle, individuals can potentially enhance their HRV, contributing to better overall health and well-being.
The Connection Between HRV and the Autonomic Nervous System
The importance of HRV lies in its ability to reflect the balance within the autonomic nervous system, particularly between the sympathetic and parasympathetic branches. Heart rate variability indexes the oscillations in the heart and provides insights into how many times your heart beats in response to various stimuli. The role of heart rate variability is crucial in understanding the rate variability and cardiac vagal tone, which is a key component of heart rate variability.
How to Measure Heart Rate Variability Effectively?
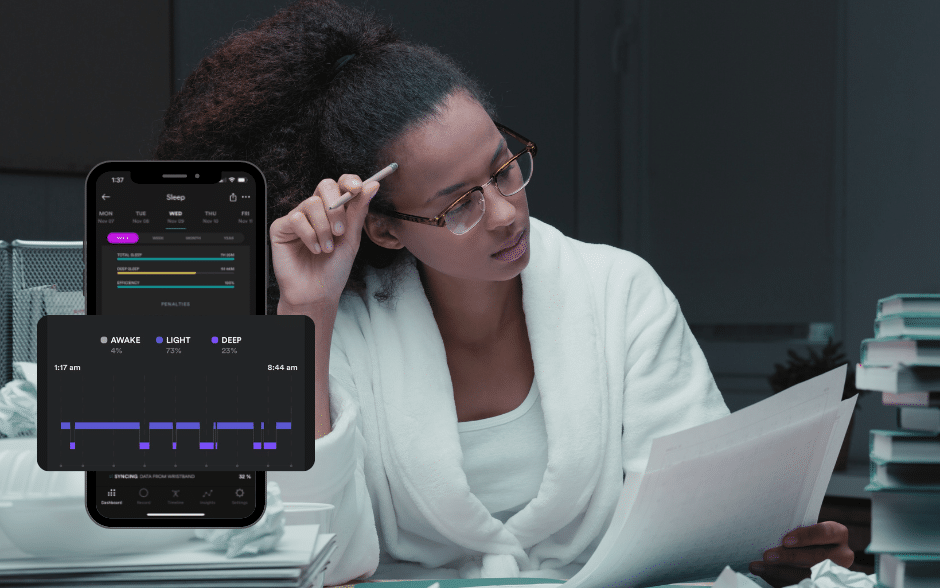
It’s important to use a reliable device and ensure that the context of your measurement is consistent. Biostrap, as an example, offers advanced, clinical-grade sensors that can capture accurate HRV readings, making it an excellent choice for monitoring HRV.
- Use a Reliable Device: Devices like Biostrap are equipped with precise sensors that measure HRV through photoplethysmography (PPG). Accurate readings from devices like this help ensure that the data you’re collecting is meaningful and reflective of your true autonomic function.
- Measure During Rest: The context of when and how you measure HRV is critical. To get accurate readings, measure HRV when your body is calm, such as after waking up or during a relaxed state. Biostrap’s Spot Check feature can be used during these times to capture a stable HRV reading, giving insight into your body’s resting state and parasympathetic activity.
- Consistency is Key: HRV can fluctuate throughout the day based on factors like stress, activity, and hydration. For consistent results, take measurements at the same time every day, in similar conditions. For example, using Biostrap each morning after a good night’s sleep provides a reliable baseline, whereas measuring during a stressful moment might lead to an artificially low HRV.
- Track HRV Trends Over Time: Short-term fluctuations are normal, but the power of HRV measurement comes from observing long-term trends. Devices like Biostrap allow you to monitor your HRV data over weeks or months, giving you a better understanding of your overall heart health and how factors like exercise, diet, and stress management affect your autonomic balance.
- Context Matters: HRV is highly influenced by context, such as whether you’re in a resting state or during physical activity. Measuring HRV during or right after a workout can show a low HRV, as your sympathetic nervous system is activated. However, measuring at rest, such as using Biostrap when relaxed, will provide a more accurate assessment of your parasympathetic recovery state.
- Analyze with HRV Metrics: The Biostrap app offers a comprehensive analysis of your HRV, including metrics like RMSSD and SDNN. These metrics are important for understanding your short-term and long-term HRV, providing insights into how well your body is managing stress and recovery.
Heart Rate Variability Parameters
Various methods exist to measure HRV using different analytical approaches, each providing unique insights into the variability and heart rate dynamics. The methods are listed below.
Time Domain
Time domain measures focus on the variation in time intervals between successive heartbeats, known as R-R intervals or NN intervals (normal-to-normal heartbeats). These are the simplest HRV measurements and are widely used to assess the overall level of autonomic activity, particularly the parasympathetic nervous system’s influence on heart rate.
Common time domain metrics:
- SDNN: Standard deviation of all NN intervals, indicating overall HRV. Higher values reflect greater variability and a healthier balance between the sympathetic and parasympathetic nervous systems.
- RMSSD: Root mean square of successive differences between NN intervals, primarily reflecting short-term HRV influenced by the parasympathetic nervous system.
- pNN50/NN50: Percentage or count of successive NN intervals that differ by more than 50 ms, indicative of short-term vagal (parasympathetic) activity.
Higher time domain values generally indicate better heart health, higher parasympathetic activity, and better stress recovery. Lower values can signal stress, fatigue, or chronic conditions.
Frequency Domain
Frequency domain analysis breaks down the R-R intervals into different frequency bands using spectral analysis (usually via Fast Fourier Transform or autoregressive modeling). Each frequency band is associated with specific components of autonomic regulation.
Common frequency domain metrics:
- VLF (Very Low Frequency, <0.04 Hz): Represents slow regulatory mechanisms, possibly reflecting thermoregulation and long-term regulation.
- LF (Low Frequency, 0.04-0.15 Hz): Represents both sympathetic and parasympathetic activity, though it is often linked more closely with sympathetic modulation.
- HF (High Frequency, 0.15-0.4 Hz): Reflects parasympathetic or vagal activity, often associated with respiratory cycles (respiratory sinus arrhythmia).
- LF/HF Ratio: A commonly used measure to assess the balance between sympathetic (LF) and parasympathetic (HF) activity. A higher ratio may indicate increased sympathetic nervous system dominance, while a lower ratio indicates parasympathetic dominance.
Frequency domain measures provide a deeper look into the balance of autonomic activity over time. High HF values suggest strong parasympathetic activity, while high LF values suggest either increased sympathetic or both sympathetic and parasympathetic activity. The LF/HF ratio is often used to assess autonomic balance, but its interpretation is context-dependent.
Non-linear Domain
Non-linear analysis looks at HRV from the perspective of chaos theory and complexity. It assesses the unpredictability and variability in heart rate patterns over time, providing insights into the autonomic nervous system’s flexibility in adapting to stressors.
- Common non-linear domain metrics:
- Poincaré Plot: A graphical representation of the relationship between successive R-R intervals, showing both short-term and long-term variability.
- SD1: Measures short-term HRV, corresponding to parasympathetic activity.
- SD2: Measures long-term HRV, associated with the overall variability.
- Sample Entropy (SampEn) and Approximate Entropy (ApEn): Measures the complexity and irregularity of heart rate fluctuations. Higher entropy reflects greater variability and adaptability.
- DFA (Detrended Fluctuation Analysis): Assesses fractal-like correlation properties in HRV, reflecting long-term regulatory mechanisms.
Non-linear metrics provide a deeper understanding of how adaptive and flexible the autonomic nervous system is. Higher complexity (e.g., high entropy) suggests a robust, adaptive cardiovascular system, while lower values can indicate poor adaptability and increased risk for cardiovascular problems.
Geometric Domain
Geometric methods assess HRV by creating geometrical representations of R-R interval distributions, typically through histograms or other graphical plots.
- Common geometric domain metrics:
- HRV Triangular Index: Measures the total number of NN intervals divided by the height of the frequency distribution of all NN intervals. It reflects overall HRV and is sensitive to both short- and long-term changes in variability.
- TINN (Triangular Interpolation of NN Interval Histogram): The width of the base of the RR interval histogram, indicating overall variability.
Geometric methods give a broad view of HRV, emphasizing long-term trends in variability. These metrics are particularly useful in clinical settings for assessing overall heart health and risk stratification.
Which HRV method is better?
The choice of method for measuring HRV varies depending on the specific aspect of autonomic function being investigated. Each method offers distinct advantages and limitations, contributing to a holistic understanding of heart rate variability among different populations and clinical conditions.
While RMSSD has taken the stage as the most popular HRV parameter, there are over 50 various HRV measurements used in clinical psychology as shown in the table below.
| HRV Parameter |
Description |
Domain |
| Mean RR |
Average time between successive R-R intervals |
Time |
| SDNN |
Standard deviation of NN intervals |
Time |
| RMSSD |
Root mean square of successive differences between adjacent RR intervals |
Time |
| pNN50 |
Percentage of successive RR intervals differing by more than 50 ms |
Time |
| NN50 |
Number of successive RR intervals differing by more than 50 ms |
Time |
| SDANN |
Standard deviation of the average of NN intervals in 5-minute segments |
Time |
| HR Max – HR Min |
Difference between maximum and minimum heart rate |
Time |
| Triangular Index |
Integral of the density distribution of RR intervals divided by the height of the histogram |
Geometric |
| TINN |
Baseline width of the RR interval histogram |
Geometric |
| LF |
Power in low-frequency range (0.04-0.15 Hz) |
Frequency |
| HF |
Power in high-frequency range (0.15-0.4 Hz) |
Frequency |
| VLF |
Power in very low-frequency range (0.0033-0.04 Hz) |
Frequency |
| ULF |
Power in ultra-low-frequency range (<0.0033 Hz) |
Frequency |
| LF/HF Ratio |
Ratio of LF to HF power, indicating sympathovagal balance |
Frequency |
| Total Power |
Total power of all spectral components |
Frequency |
| ApEn |
Approximate entropy, measures the complexity or irregularity in data |
Non-linear |
| SampEn |
Sample entropy, an improvement over ApEn for measuring irregularity |
Non-linear |
| DFA |
Detrended fluctuation analysis, assesses fractal correlations in RR intervals |
Non-linear |
| Baevsky Stress Index |
A geometric measure of HRV that reflects the stress experienced by the cardiovascular system |
Geometric |
| Poincaré SD1 |
Short-term HRV, ellipse perpendicular to the line of identity in the Poincaré plot |
Geometric |
| Poincaré SD2 |
Long-term HRV, ellipse along the line of identity in the Poincaré plot |
Geometric |
| Shannon Entropy |
Measures the unpredictability of RR intervals |
Non-linear |
| LFnu |
Normalized low-frequency power |
Frequency |
| HFnu |
Normalized high-frequency power |
Frequency |
| CVRR |
Coefficient of variation of RR intervals |
Time |
| CSI (Cardiac Sympathetic Index) |
A ratio indicating sympathetic activity |
Geometric |
| CVI (Cardiac Vagal Index) |
A ratio indicating parasympathetic activity |
Geometric |
| RR Triangular Index |
Measure of overall HRV based on the distribution of RR intervals |
Geometric |
| HF Peak Frequency |
Frequency at which the peak power of the HF band occurs |
Frequency |
| LF Peak Frequency |
Frequency at which the peak power of the LF band occurs |
Frequency |
| ULF Peak Frequency |
Frequency at which the peak power of the ULF band occurs |
Frequency |
| VLF Peak Frequency |
Frequency at which the peak power of the VLF band occurs |
Frequency |
| Lyapunov Exponent |
Measure of the rate of separation of infinitesimally close trajectories |
Non-linear |
| Correlation Dimension |
Estimates the dimensionality of RR intervals |
Non-linear |
| Multiscale Entropy |
Measures complexity across multiple scales |
Non-linear |
| Fractal Dimension |
Measures self-similarity in HRV data |
Non-linear |
| SDRR |
Standard deviation of RR intervals |
Time |
| NN20 |
Number of successive RR intervals differing by more than 20 ms |
Time |
| pNN20 |
Percentage of successive RR intervals differing by more than 20 ms |
Time |
| Skewness |
Measures asymmetry in the RR interval distribution |
Non-linear |
| Kurtosis |
Measures the “tailedness” of the RR interval distribution |
Non-linear |
| Log Power |
Logarithmic transformation of total power |
Frequency |
| Relative LF Power |
LF power relative to total power |
Frequency |
| Relative HF Power |
HF power relative to total power |
Frequency |
| Relative VLF Power |
VLF power relative to total power |
Frequency |
| Deceleration Capacity |
Measures deceleration in heart rate, associated with vagal tone |
Time/Non-linear |
Using a Heart Rate Variability Monitor for Accurate Results
Utilizing a reliable and clinical-grade Heart Rate Variability Monitor, such as the Biostrap Kairos, offers a sophisticated method for obtaining accurate results in assessing cardiovascular health.
To obtain accurate R-R intervals from PPG data for HRV analysis, it’s essential to filter out noise and artifacts that can interfere with signal quality. Motion artifacts, sensor placement, and external interference can cause disruptions in PPG signals, so applying band-pass filtering helps isolate the frequency range associated with heartbeats. Advanced noise reduction techniques, like adaptive noise cancellation or Kalman filtering, are used to remove unwanted noise from movement or environmental factors. Additionally, accurate peak detection is necessary to identify true heartbeats and avoid confusing features like the dicrotic notch in the pulse waveform.
Once the signal is processed, artifact correction plays a crucial role in ensuring clean data. Motion or stress-induced outliers can be filtered out using statistical techniques, and signal reconstruction methods, such as spline interpolation, can fill in gaps where noise has corrupted the signal. Using adaptive algorithms that adjust to dynamic conditions, such as changes in physical activity or body movement, ensures consistency in R-R interval detection across different states.
Lastly, it’s important to measure HRV in appropriate contexts, such as during rest, to avoid artificially low readings caused by sympathetic nervous system activation during exercise or stress. By applying these filtering techniques and carefully managing the measurement context, PPG-derived HRV data can be made more reliable and accurate, comparable to ECG in many cases.
You can track your HRV with clinical reliability with the Biostrap wrist-worn device and keep an eye on your nocturnal HRV as well as weekly, monthly and yearly trends.
What Factors Influence Heart Rate Variability?
Several factors influence heart rate variability, including age, physical fitness, and lifestyle choices. As individuals age, there is a natural decline in HRV, which may be attributed to the reduced elasticity of the heart and blood vessels, as well as changes in autonomic function. Conversely, regular physical activity and a healthy lifestyle can enhance HRV by improving cardiovascular efficiency and autonomic balance.
Psychological stress and emotional well-being also significantly impact heart rate variability. Chronic stress and anxiety can lead to a reduction in HRV, indicating a dominance of the sympathetic nervous system over the parasympathetic system. This imbalance may result in increased heart rate and reduced adaptability to environmental changes. Conversely, practices such as meditation and mindfulness can enhance HRV by promoting relaxation and parasympathetic activation.
Moreover, sleep quality and duration are vital determinants of heart rate variability. Poor sleep can lead to low HRV, suggesting impaired recovery and heightened stress levels. Differences in heart rate during sleep cycles are essential for restoring autonomic balance and ensuring optimal cardiovascular health.
The Impact of the Sympathetic Nervous System on HRV
The sympathetic nervous system plays a significant role in reducing heart rate variability (HRV) by activating the body’s “fight or flight” response during times of stress. When the sympathetic system is dominant, it increases heart rate and reduces the body’s ability to relax, leading to a lower HRV.
How the Parasympathetic Nervous System Affects HRV
The parasympathetic nervous system has a positive effect on heart rate variability (HRV) by promoting relaxation and recovery in the body. When the parasympathetic system is active, it slows down the heart rate and allows the body to enter a calm state, which increases HRV.
External Factors that Can Influence HRV
Several external factors can significantly influence heart rate variability (HRV).
- Stress: Activates the sympathetic nervous system, reducing HRV.
- Physical Activity: Regular exercise improves HRV long-term, but intense exercise can temporarily lower HRV.
- Sleep Quality: Poor sleep decreases HRV, while good sleep boosts parasympathetic nervous system activity and increases HRV.
- Diet:
- Alcohol and caffeine can lower HRV by increasing sympathetic nervous system activity.
- A diet rich in omega-3 fatty acids supports higher HRV.
- Hydration: Dehydration reduces HRV by straining cardiovascular function.
- Temperature Extremes: Exposure to heat or cold can stress the body and temporarily reduce HRV.
- Emotional State: Positive emotions increase HRV, while negative emotions and anxiety can lower HRV.
- Medication: Some medications, especially those affecting the cardiovascular or autonomic systems, can impact HRV levels.
How to Increase Heart Rate Variability for Better Health?
Techniques to Increase HRV Naturally
Here are several science-backed techniques that have been shown to increase Heart Rate Variability (HRV) naturally.
1. Mindfulness Meditation
Mindfulness meditation promotes relaxation by focusing on the present moment, which activates the parasympathetic nervous system. Regular practice has been shown to reduce stress and increase HRV, helping balance the autonomic nervous system by reducing sympathetic dominance and enhancing vagal tone.
2. Deep Breathing (Slow and Diaphragmatic)
Slow, controlled breathing, especially at a rate of around 5-6 breaths per minute, stimulates the vagus nerve, improving parasympathetic activity. This method naturally increases HRV by helping the body transition from a stressed state to a relaxed, restorative state.
3. Physical Exercise
Moderate, consistent aerobic exercise boosts cardiovascular health and enhances autonomic balance, leading to long-term increases in heart rate variability and improved influence on HRV. Exercise strengthens parasympathetic modulation and reduces sympathetic nervous system overactivity, particularly when combined with proper recovery.
4. Good Sleep Hygiene
High-quality sleep is essential for autonomic recovery and improving HRV. Ensuring sufficient, uninterrupted sleep allows the body to restore balance between the sympathetic and parasympathetic nervous systems, leading to higher HRV during waking hours.
5. Cold Exposure
Cold showers or ice baths can stimulate the vagus nerve, activating the parasympathetic system and increasing HRV. Short, controlled exposure to cold can enhance autonomic resilience and improve the body’s ability to switch between sympathetic and parasympathetic states.
6. Balanced Diet with Omega-3 Fatty Acids
A diet rich in omega-3 fatty acids (found in fish, nuts, and seeds) supports heart health and reduces inflammation, leading to improvements in HRV. Omega-3s help balance the autonomic nervous system by enhancing parasympathetic tone.
7. Yoga and Tai Chi
These practices combine movement, breathing, and mindfulness, which together increase parasympathetic activity and HRV. Regular participation in yoga or tai chi helps the body maintain a balanced autonomic nervous system, reducing stress and improving heart function.
8. Biofeedback Training
Biofeedback devices allow individuals to monitor and consciously control their HRV. Through guided breathing and relaxation techniques, users can learn to regulate their autonomic nervous system, improving their HRV by promoting parasympathetic activation.
9. Reducing Alcohol and Caffeine Intake
Alcohol and caffeine can reduce HRV by overstimulating the sympathetic nervous system. Reducing consumption of these substances helps maintain autonomic balance, allowing parasympathetic activity to recover and HRV to increase naturally.
10. Positive Social Connections
Meaningful interactions with friends and loved ones can reduce stress and improve HRV. Positive social bonds promote emotional well-being, which activates the parasympathetic nervous system, helping to enhance heart rate variability.
11. Laughter and Positive Emotions
Experiencing joy and laughter activates the parasympathetic nervous system, reducing stress and increasing HRV. Positive emotions contribute to greater autonomic balance, helping the body recover from stress more efficiently.
Each of these methods has been scientifically shown to support autonomic health, helping to increase HRV naturally by promoting parasympathetic activity and reducing the effects of stress.
12. Hydration
Dehydration can strain the heart, increase sympathetic activity, and reduce HRV by making it harder for the body to regulate temperature, blood flow, and overall physiological balance. Staying well-hydrated helps the body maintain a healthy balance between sympathetic and parasympathetic activity, supporting optimal heart function and improving HRV. Drinking enough water throughout the day is a simple yet effective way to promote autonomic balance and enhance overall well-being.
The Role of HRV Biofeedback in Health Improvement
HRV biofeedback is a powerful tool for improving health by providing real-time insights into the balance between the sympathetic and parasympathetic nervous systems. By using biofeedback devices, individuals can monitor their heart rate variability (HRV) and learn to control their breathing, stress responses, and autonomic function. Through this process, users can increase high heart rate variability, promoting a healthier resting heart rate and better regulation of heart rate and blood pressure. Studies show that HRV biofeedback can reduce stress, enhance emotional resilience, and improve cardiovascular health, making it particularly beneficial for those at risk of coronary heart disease or heart failure. Over time, regular HRV biofeedback training can lead to lasting improvements in overall well-being and heart function, as it helps individuals strengthen their parasympathetic nervous system and improve their body’s response to stress.
Understanding the Benefits of a Higher HRV
A higher Heart Rate Variability (HRV) is a strong indicator of a healthy, adaptable heart and balanced autonomic nervous system, reflecting the balance between the sympathetic nervous system (fight or flight) and the parasympathetic nervous system (rest and digest). When HRV is high, it suggests that the heart is responsive to changes in stress, activity, and rest, leading to better regulation of heart rate and blood pressure. Conversely, low HRV or low heart rate variability is often linked to health risks such as coronary heart disease, heart failure, and poor cardiovascular resilience. By increasing HRV through healthy lifestyle choices, individuals can promote heart health, reduce the risk of heart failure, and improve overall well-being.
What are the Implications of Low Heart Rate Variability?
Health Risks Associated with Low Heart Rate Variability
A low heart rate variability is linked to several serious health risks, particularly involving the heart. It is a strong predictor of congestive heart failure, coronary heart disease, and increased mortality. When the HRV index is consistently low, the body’s ability to regulate stress is compromised, leading to poor long-term health outcomes. Heart rate variability in patients with chronic conditions tends to decrease, signaling deteriorating autonomic function. This can further complicate recovery and increase the likelihood of experiencing cardiovascular events like heart attacks or strokes.
Frequently Asked Questions
1. What is a good heart rate variability?
Heart Rate Variability values are highly individual, and what’s considered “good” varies from person to person. Marco Altini points out that it’s more important to focus on personal trends rather than comparing absolute HRV values with others. A higher HRV generally indicates better autonomic nervous system balance and cardiovascular health for an individual, but personal baselines are key to meaningful interpretation.
2. Can tracking HRV help in managing stress and improving recovery?
Yes, monitoring HRV can be a valuable tool for managing stress and enhancing recovery. Andrew Flatt emphasizes that fluctuations in HRV reflect changes in autonomic nervous system activity. A decrease in HRV may signal increased stress or inadequate recovery, suggesting the need for rest or stress-reduction strategies. By keeping an eye on HRV trends, individuals can make informed decisions to adjust their lifestyle, optimize recovery, and maintain overall well-being.
3. How does HRV change with age and fitness level?
HRV generally decreases with age due to reduced autonomic nervous system flexibility. Marco Altini notes that regular physical activity can help maintain higher HRV levels, as fitness enhances cardiovascular health and autonomic function. Physically active individuals often exhibit higher HRV compared to sedentary peers.
4. Can HRV be used to detect overtraining in athletes?
Yes, HRV monitoring can identify signs of overtraining. Andrew Flatt emphasizes that a consistent drop in HRV may indicate inadequate recovery and accumulated fatigue. By tracking HRV, athletes can adjust their training intensity to prevent overtraining and reduce the risk of injury.
5. What factors can influence HRV measurements?
Various factors affect HRV, including stress, sleep quality, hydration, and time of day. Marco Altini advises measuring HRV under consistent conditions, preferably in the morning, to obtain reliable data. Being aware of these factors helps in accurately interpreting HRV trends.
6. Is HRV monitoring useful for mental health management?
HRV is linked to stress and emotional regulation. Andrew Flatt suggests that tracking HRV can provide insights into an individual’s stress levels and psychological well-being. Higher HRV is associated with better stress resilience, while lower HRV may signal increased stress or anxiety.
7. How can HRV biofeedback improve health outcomes?
HRV biofeedback training involves exercises that enhance autonomic control and increase HRV. Marco Altini explains that such practices can reduce stress, improve heart health, and promote relaxation. Biofeedback is a tool that can support overall well-being when incorporated into regular routines.
8. What is the relationship between HRV and sleep quality?
Quality sleep positively impacts HRV. Andrew Flatt notes that sufficient and restful sleep promotes autonomic balance, leading to higher HRV readings. Poor sleep can decrease HRV, indicating heightened stress and inadequate recovery.
9. Can HRV help in managing chronic diseases?
Monitoring HRV may assist in managing conditions like hypertension and diabetes. Marco Altini points out that lower HRV is often associated with chronic diseases due to autonomic dysfunction. Regular HRV tracking can help assess disease progression and the effectiveness of treatments.
10. Are wearable devices accurate for measuring HRV?
Wearable devices have made HRV monitoring more accessible, but accuracy varies. Andrew Flatt recommends using validated devices and following standardized protocols for consistency. While convenient, it’s important to interpret wearable HRV data cautiously and consider potential limitations.
11. How high can heart rate variability go?
In adults, heart rate variability (HRV) typically spans from less than 20 milliseconds to in excess of 200 milliseconds. Nonetheless, HRV is subject to individual differences and is affected by numerous factors, such as age, gender, physical fitness, and genetic predispositions.