Respiratory rate is one of the main vital signs that measure a person’s health. Alongside body temperature, blood pressure, heart rate, respiratory rate is an essential measurement for determining well-being.
Respiratory rate is the rate at which a full breathing cycle occurs, both inhalation and exhalation. While this is something that can be taken over by voluntary control, the majority of respiratory rate is an autonomic process, which occurs as a result of many inputs, including the respiratory center of the brain, which sends physiological sensory information throughout the body.
Age, weight and certain illnesses can all influence a person’s respiration rate. That’s why your normal respiratory rate may differ from the next person’s. If you learn to measure your respiratory rate, you’ll gain a better understanding of what is normal for you.
What Is a Normal Respiratory Rate?
The normal ranges for respiratory rate vary depending on a number of factors. For example, people who regularly practice deep breathing exercises, or those who play woodwind instruments, may take less breaths per minute, whereas people who are less physically fit may take more breaths per minute.
“We don’t really believe in comparing someone to a normal curve,” explains Kevin Longoria, MSc, a clinical exercise physiologist and the Chief Science Officer for Biostrap. “More importantly, we believe in comparing them to themself. We can see what someone’s normal respiratory rate may be and establish a trend. Then, you look at changes in the trend.” This allows you to determine what is a normal respiratory rate and what is abnormal for you as an individual.
In general, an abnormal respiratory rate is when the number of breaths per minute is under 12 or over 25 — but again, this can vary for every individual. A high respiratory rate means that the respiratory system is being overworked when it circulates oxygen through the blood and body. Conditions like asthma or sudden episodes, like an anxiety attack, can increase the number of times a person breathes per minute, resulting in a high respiratory rate.
In contrast, a child’s breathing rate would be different. “The normal respiratory rate changes significantly throughout the first several years of a child’s development,” says Longoria. For example, a baby up to 6-month old will usually have a breathing rate between 30 and 60 breaths per minute. A child between one and five will usually have a breathing rate between 20 and 30. By the time a child is 12, their breathing rate will usually be under 20.
According to Longoria, “abnormally high respiratory rates in children may be a sign of fever, dehydration, or conditions including bronchiolitis or pneumonia. Children may also experience rapid respiratory rates similar to adults due to other medical conditions including acidosis (with diabetes) and asthma.” And these are just a few of the factors that influence respiratory rate.
Factors That Influence Respiratory Rate
There are a number of common conditions that influence a person’s respiratory rate. For example, having anxiety and suffering from panic attacks can result in shallow breathing patterns and an acutely high respiratory rate for a short period of time (also referred to as hyperventilation).
“What’s really important when you look at respiratory rate is understanding autonomic control,” says Longoria. “When we look at the autonomic nervous system, it’s controlling all these voluntary processes like heart rate, respiratory rate, response to exercise, stress hormones, inflammatory processes — essentially things we don’t have to think about.” Factors such as exercise, stress, or changes in heart rate can influence respiratory rate involuntarily.
Shallow breaths or hyperventilation could be caused by the following conditions.
Lung and Airway Diseases
Lung diseases cause reduced oxygen uptake and prevent the lungs from working properly. For example, emphysema, severe/refractory asthma, and chronic bronchitis block a person’s airflow and contribute to an increasing sense of breathlessness.
These diseases are classified under the term Chronic Obstructive Pulmonary Disorder (COPD). Symptoms include shortness of breath, wheezing, chest tightness and chronic cough with and without mucus. COPD is primarily caused by smoking cigarettes but can also be associated with genetic conditions.
When it comes to factors that influence respiratory rate, “smoking is an obvious one,” notes Longoria. “If you’re smoking, then you’re getting more tar buildup and essentially causing what’s called a respiratory restriction.” Tar buildup in the lungs will damage your air sacs (alveoli) where gas diffusion takes place. “If we’re limiting the surface area of our lungs, our body will have to compensate with a higher respiratory rate.”
Having COPD is a risk indicator of cardiac arrest, in which the heart suddenly stops beating. Sudden cardiac arrest is a medical emergency that requires immediate treatment with a defibrillator. According to Harvard Medical School, more than 13 million Americans have COPD, and it tends to coexist with other conditions, like heart disease. Yet, many people are unaware of COPD.
Anyone who suspects they have COPD can be diagnosed by a spirometry test. This is a simple non-invasive process that evaluates your exhalation to see how well your lungs are working.
Sleep Disorders
Sleep disorders are another leading cause of airway obstruction and respiratory irregularities. During non-REM sleep, the part of our sleep cycle in which we spend 80% of the night, it’s normal to breathe slowly and steadily.
Breathing normally increases and decreases through different sleep stages, and the number of breaths a person takes will vary. However, having a sleep disorder can cause irregular sleep patterns and contribute to respiratory abnormalities. One example is sleep apnea, a common sleep disorder where a person stops breathing for as much as several seconds in their sleep.
Heart Conditions
Heart problems can also affect a person’s respiratory rate. For example, atrial fibrillation (marked by irregular and rapid heart rate) can cause shortness of breath. When your heart beats irregularly due to atrial fibrillation, you may experience a tight chest and shortness of breath because the heart’s electrical signals don’t fire properly.
Cardiovascular Fitness
Cardiovascular fitness is defined as the ability of your heart and lungs to deliver oxygen-rich blood to muscles throughout the body. “If you are frequently exercising, you tend to maintain better lung volume, resting lung capacity, and you have more arterial elasticity,” says Longoria. “Per breath, you’re consuming more oxygen than the next guy.” As a result, your respiratory rate will be lower because it will require fewer breaths to consume the same amount of oxygen.
How to Measure Respiratory Rate
Understanding your respiratory rate can make you more familiar with your body and help you monitor changes as you age. Plus, it can ensure that you recognize when it might be time to consult a medical professional about any changes to your body if changes to your respiratory rate occur.
Respiratory rate can be measured through photoplethysmography (PPG) by measuring the baseline shifts that occur with breathing. The baselines move up and down in an oscillatory pattern, which corresponds to the breath cycle.
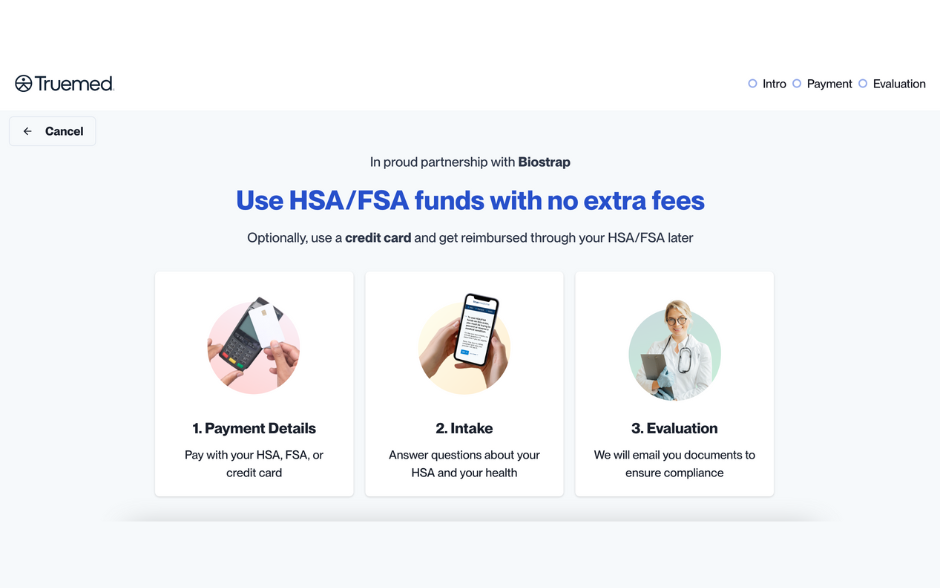
A way to use PPG to measure is through a wearable that tracks vital biometrics for both sleep and fitness like Biostrap. “Biostrap is the only clinically-validated sensor system out there,” says Longoria. Wearable trackers can measure your oxygen saturation to indicate how much oxygen is pumping through the blood. It also helps you monitor the effectiveness of your workouts to better understand how blood oxygen levels could be increased through exercise, diet, deep breathing, and other healthy lifestyle changes.
Knowing Your Respiratory Rate
Your respiratory rate tells how much oxygen is flowing through your blood, but it also provides deeper clues to your health. For example, an abnormal respiratory rate can shed light on potential sleep disorders, lung disease, and heart conditions. “It’s an extremely important biometric,” Longoria stresses. “But it’s almost more important to know how and when you’re measuring it.”
Respiratory rate helps us understand changes in our own bodies, especially as we age or try out new approaches to fitness. Measuring your respiratory rate with a wearable that measures and tracks vital biometrics for both sleep and fitness can ensure that you’re always in tune with your body and the breath that keeps it alive.