Sympathetic Arousal and Heart Rate Variability
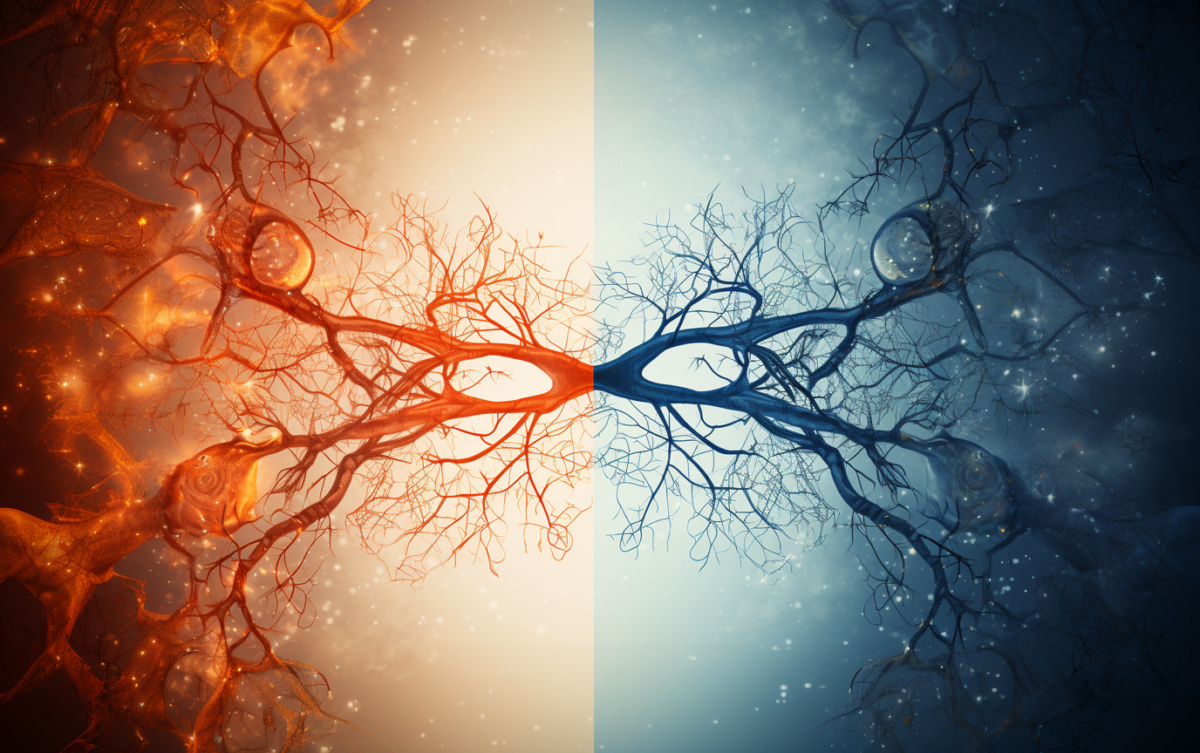
Understanding mental health and stress management is crucial for clinics aiming to improve patient care and deliver better mental health outcomes. Two critical metrics in this area are Heart Rate Variability (HRV) and Sympathetic Arousal (SA). HRV measures the variation in time between consecutive heartbeats, reflecting the balance between the sympathetic and parasympathetic branches of the autonomic nervous system (ANS). The parasympathetic system helps the body relax and recover, while the sympathetic system prepares the body for action, often called the “fight or flight” response.
Parasympathetic vs Sympathetic Branch
Assessing the parasympathetic branch through short term HRV is relatively straightforward as it involves analyzing the time-domain (e.g., RMSSD) and frequency-domain (e.g., high-frequency power) components of heart rate signals. Short term HRV represents a complex relationship between the sympathetic and parasympathetic systems (Shaffer, 2017). This influence is generally consistent and can be easily isolated, making it more straightforward to evaluate ”rest and digest’ activities compared to the complexities of measuring the sympathetic system.
While HRV can provide some insights into the body’s autonomic function, it is not a reliable marker for directly assessing sympathetic arousal, or the body’s response to stress. Measuring the sympathetic side of the ANS is challenging because its signals often overlap with parasympathetic signals and are highly variable. The sympathetic nervous system (SNS) triggers rapid physiological changes in response to stress, such as increased heart rate, vasoconstriction, and heightened alertness. Unlike the parasympathetic system, which can be measured under controlled conditions, sympathetic activation is dynamic, context-sensitive, and transient. These rapid, variable responses are difficult to capture consistently using HRV alone, as HRV lacks the specificity to distinguish between sympathetic and parasympathetic contributions in real-time.
Introducing Sympathetic Arousal
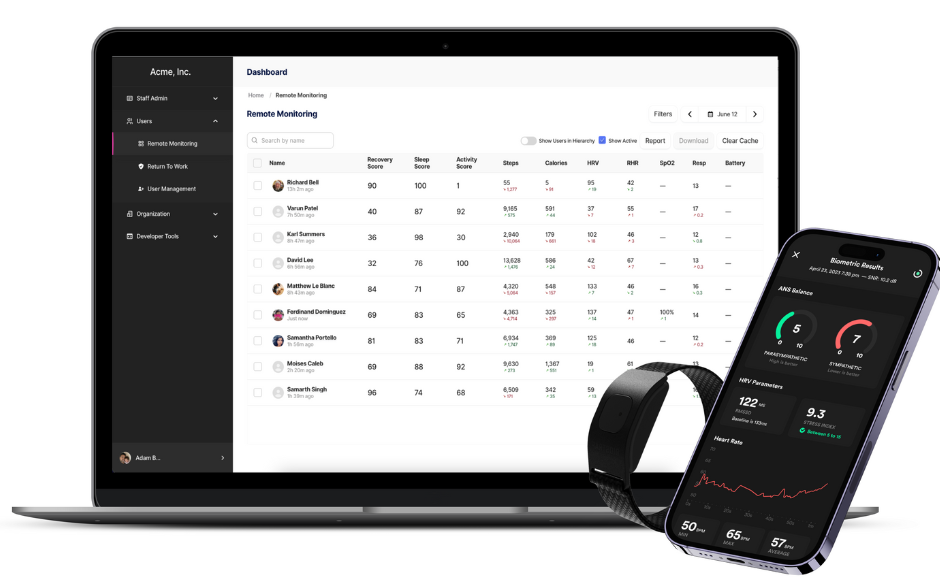
We introduce Sympathetic Arousal (SA), a precise and sensitive marker for real-time stress and anxiety management. SA provides targeted insights into stress responses, enabling timely interventions for well-being. Clinics can use SA to track, understand, and respond to patient stress, leading to more effective treatments and improved mental health outcomes.
How is Sympathetic Arousal Measured?
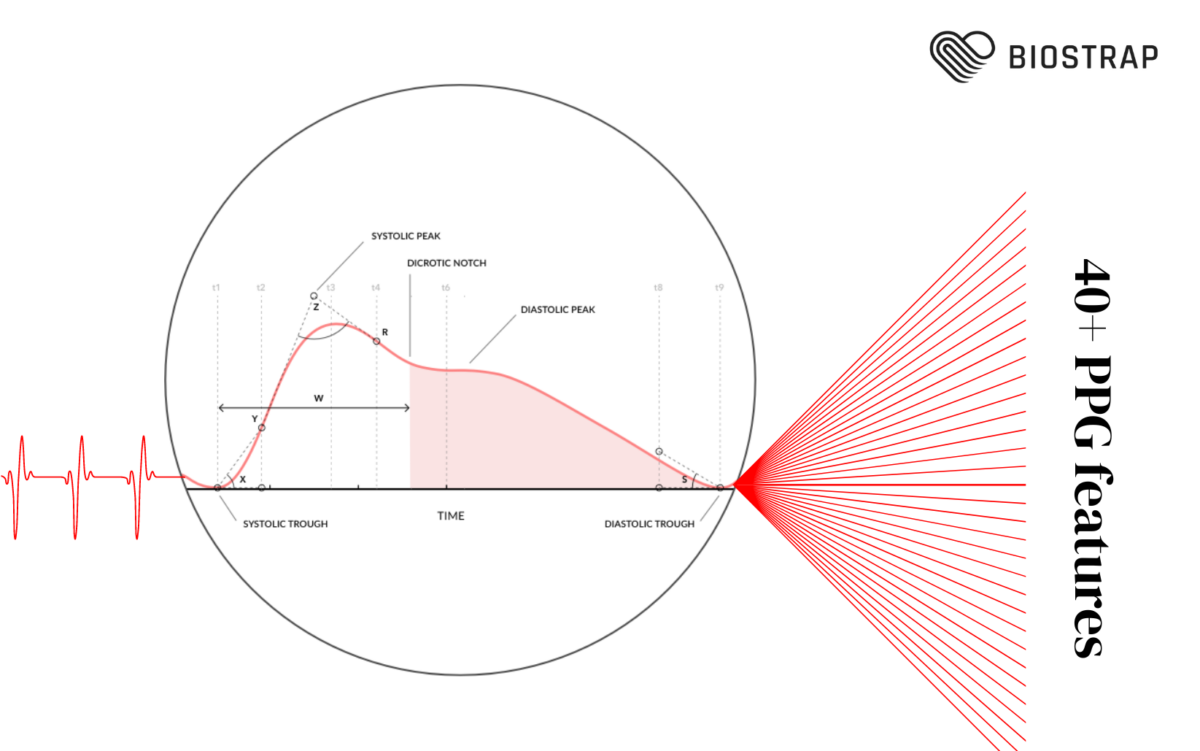
During stress or excitement, the body’s nervous system causes the tiny blood vessels in your skin to tighten, reducing blood flow. This is part of the “fight or flight” response, preparing the person for action by sending more blood to the muscles and heart. When you’re calm, your skin gets more blood flow, and when you’re stressed, less blood flows to the skin. This change in blood flow can be used to measure how stressed or emotionally aroused a person is—this is the essence of Sympathetic Arousal measurement.
We are excited to have partnered with Philia Labs, developer of a cutting-edge AI-powered algorithm using Biostrap’s high-definition PPG Waveshape features to track these subtle changes in blood to measure Sympathetic Arousal.
This algorithm has been trained on stressor timings (Udhayakumar et al, 2023) and microneurography (Rahman et al 2024, under review) , a gold-standard technique that records real-time nerve activity by inserting a microelectrode into a peripheral nerve. This invasive method directly measures the signals in the sympathetic and parasympathetic nerves, offering precise insights into the autonomic nervous system’s activity. By leveraging this AI-driven measurement method, we can access previously unattainable insights with HRV alone.
Measuring Sympathetic Arousal and HRV Together
By combining HRV and Sympathetic Arousal measurements, clinics gain a more comprehensive understanding of physical and emotional stressors affecting their patients. This dual approach enables earlier interventions and more personalized wellness plans, which can translate into better patient outcomes and overall mental health improvement. Key benefits include:
- Detecting early signs of chronic stress and anxiety by identifying physiological changes that are linked to prolonged stress responses. This is key for preventing burnout and maintaining employee well-being.
- Providing more accurate mental health assessments beyond HRV.
- Identifying specific stress triggers for better management and coping strategies, allowing clinics to understand what stressors may lead to heightened arousal in patients and adjust treatment plans accordingly.
- Removing guesswork from evaluating intervention efficacy by objectively measuring changes in sympathetic and parasympathetic arousal. Improvements in sympathovagal balance can ensure that treatment efforts are making an impact on health and well-being outcomes.
- Benchmarking best practices for increased ROI by determining which wellness strategies provide the most effective reduction in stress and improving overall employee outcomes.
Monitoring Fatigue
Fatigue is a state of physical or mental exhaustion that results from prolonged activity, stress, or lack of rest. It can manifest as reduced energy levels, impaired concentration, and diminished physical or cognitive performance due to prolonged sympathetic dominance (Tanaka, 2015). Benefits of monitoring both HRV and Sympathetic Arousal can be helpful for fatigue in the following ways:
- Spotting physical and mental exhaustion patterns early, allowing for proactive adjustments in workloads or daily routines.
- Tailoring fatigue management strategies at scale to improve overall well-being by creating individualized treatment plans that consider the recovery and arousal aspects of a patient’s health.
How Sympathetic Arousal Can Be Used For Your Business
Sympathetic Arousal (SA) is more than just a stress metric—it’s a powerful tool that can transform mental health care, performance optimization, and stress management across various fields.
Healthspan & Longevity Clinics: Chronic stress accelerates aging by over-activating the sympathetic nervous system, leading to inflammation, oxidative stress, cellular damage, and increased risk of age-related diseases like cardiovascular issues and cognitive decline. Monitoring Sympathetic Arousal (SA) helps detect and manage stress early, enabling healthspan clinics to create personalized plans that slow aging, enhance recovery, and promote long-term vitality for healthier, longer lives.
Elite Athletes: Stress disrupts athletic performance by impairing recovery, increasing the risk of injury, and reducing focus and endurance due to prolonged sympathetic nervous system activation. By tracking Sympathetic Arousal (SA), excessive stress can be identified, allowing athletes and coaches to optimize recovery, balance training, and minimize the risks of burnout and injury.
First Responders & Military Personnel: Chronic stress and fatigue in first responders (e.g. Police, firefighter, EMTs) and military personnel impair decision-making, reduce endurance, and heighten the risk of injury or burnout. Prolonged exposure without recovery increases vulnerability to PTSD and other mental health issues, impacting long-term resilience. By monitoring Sympathetic Arousal (SA) in real time, stress can be managed during critical operations, improving performance and reducing the long-term risks of burnout and PTSD.
References
Shaffer, F. (2017, September 28). An Overview of Heart Rate Variability Metrics and Norms. PubMed. Retrieved October 11, 2024, from https://pubmed.ncbi.nlm.nih.gov/29034226/
Tanaka, M. (2015, September 29). Frontier studies on fatigue, autonomic nerve dysfunction, and sleep-rhythm disorder. NCBI. Retrieved October 11, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621713/
Udhayakumar, R. (2023, August 30). Measurement of stress-induced sympathetic nervous activity using multi-wavelength PPG. Royal Soc. Open Science. Retrieved October 11, 2024, from https://doi.org/10.1098/rsos.221382
Ziegler, M. (2012). Chapter 61 – Psychological Stress and the Autonomic Nervous System,. Primer on the Autonomic Nervous System (Third Edition). Retrieved October 11, 2024, from https://doi.org/10.1016/B978-0-12-386525-0.00061-5