Our hearts thump steadily inside our chest ensuring we live to fight another day. How fast it beats when we sit still is called our resting heart rate (RHR). It’s a standard medical vital sign and a key measurement of health and fitness.
A quick Google search for normal resting heart rate will tell you: “A normal resting heart rate for adults ranges from 60 to 100 beats a minute.” But what if what we thought we knew was wrong? A quiet revolution has been taking place, and the internet is now just beginning to notice.
We take a deep dive into what makes a good Resting Heart Rate?
What’s normal?
The classic guideline for normal ranges between 60 and 100 beats per minute. The lower the better.
But it turns out that there is an immense difference between 60 and 100 beats per minute (BPM). 60 signifies health and vitality. 100 does not. Researchers now know: every increase in resting heart rate brings a heightened risk of illness and death.
The New Normal?
Back in 1992 prominent cardiology researcher David H. Spodick challenged the 60 to 100 guideline, suggesting a re-calibrated range of 50 to 90 BPM. The conventional limits were “established by consensus and never formally examined,” he said. Clinical experience led him to conclude that both figures were too high. So Spodick delved deeper: “We investigated this formally. The normal resting daytime heart rate ranges for sinus rhythm should be readjusted from 60-100 to 50-90.”
“About 50-70 beats per minute is ideal,” per WebMD, quoting cardiologist Suzanne Steinbaum, MD.
Yet 35 years later the 60 to 100 guideline persists. Even the American Heart Association (quoting the NIH) and Mayo Clinic cite 60 to 100.
Why Does it Matter?
It’s not just the high end of the range that spells trouble. New research shows every ten point increase in RHR increases your risk of illness and death, from all causes not just cardiac disease.
Ulrik Wisloff, co-author of one of the studies, explains, “The short answer is having an RHR above 85 may be very unhealthy. Keeping your resting heart rate below 70 is best.”
Mounting Research
Study after study confirms this.
A RHR of 100 can predict lowered mortality, even in healthy adults. The Canadian Journal of Cardiology reports, “elevated heart rate (90 beats/min or greater) is a risk factor, particularly for sudden cardiac death.”
In fact, a resting heart rate of more than 80 beats a minute brings a 45 percent greater risk of death from any cause. Even those with a relatively healthy RHR between 60 to 80 have an increased mortality risk (21 percent) over those with a rate below 60.
It’s not just heart trouble. A 28 year longitudinal study of 53,322 people in Texas found “a resting heart rate greater than 80 beats per minute is a strong predictor for future heart attacks, diabetes and even cancer.”
A meta review of 18 epidemiological studies showed “a mortality excess of 30% to 50% for every 20 beats/min increase” in RHR.
Cause or Effect?
Increasing evidence suggests that an elevated heart rate doesn’t just predict a higher risk. It may actually be causing it. Elevated heart rates can reduce the elasticity of the larger arteries. A high heart rate itself may be a cardiovascular risk factor. Researchers are now studying whether lowering the heart rate can reduce cardiovascular risk.
More than 32 studies prove elevated heart rate is an independent risk factor, suggesting that
lowering RHR may play a key role in the prevention of cardiovascular diseases.
It’s not just humans: “Across a wide range of mammals slower heart rates are associated with greater longevity “
Even a RHR of 76 beats per minute, well within the classic 60 to 100 BPM guidelines, may be linked to a higher risk of heart attack.
A resting heart rate of more than 80 beats a minute brings a 45 percent greater risk of death from any cause. Even those with a relatively healthy RHR between 60 to 80 had an increased mortality risk (21 percent) over those with a rate below 60.
An elevated RHR is also linked to reduce ability to perform everyday tasks in the elderly. Researchers emphasize the need for early intervention: “Because functional disability develops gradually, it is important to identify it early and take steps to delay decline, such as exercise, medication and other interventions.” Senior in this study with the highest RHR had an “80 percent increased risk of decline in their ability to do basic daily activities, and a 35 percent increased risk of decline in their ability to do more complicated daily tasks”.
Given this research, the widely quoted parameters of 60 – 100 are just plain wrong. The paradigm has shifted from “60 to 100 is normal” to “Keep your RHR as low as possible and see a doctor if it increases > 10 points”.
Elite Athletes and Resting Heart Rate
Like any muscle, the heart grows stronger with use. The stronger it becomes the more efficient it is. It can pump larger volumes of blood with less effort,Elite athletes and the tremendously fit have RHR far below 60. This signifies extreme efficiency of their cardiovascular system. Even for those of us who may not be ultra-fit, there are interventions to lower our RHR.
What Factors Affect Resting Heart Rate?
Internal
- Emotions (increase)
- Fitness (decrease)
- Activity (increases)
- Body size (increases)
- Dehydration (increases)
External
- Temperature (heat/humidity increase RHR)
- Position (increases initially when you stand up, then stabilizes)
- Medication (varies: beta blockers slow RHR, thyroid medicine can increase it)
How Can You Lower your Resting Heart Rate?
While researchers are still weighing the exact connection between an elevated RHR and poor health, it’s clear that a low resting heart rate is a desirable sign of fitness. The best way to lower your RHR is to become more fit. Exercise s the number one fix, especially aerobic movement that taxes and strengthens your heart.
Lose weight. Stop smoking. Eat healthy. Nearly every known factor to improve health will also lower your resting heart rate.
How Often Should You Measure It?
Harvard recommends that you “check your resting heart rate early and often”.
Everyone’s heart beats but not everyone’s heart beats the same way or at the same rate.
The standard measure of heart rate is beats per minute (how many times does it go thump thump thump over 60 seconds). The spacing between each beat is not uniform – that’s called heart rate variability, and it’s actually better to have MORE variability than less. That shows your heart is capable of adjusting to changing stimuli inside and outside your body.
Our heart beats is that it varies wildly over the course of the day depending on whether we are still, active, calm, agitated or asleep.
So when it comes to measuring our heart rate, for purposes of accuracy and uniformity we measure it when we are at rest. We’ve been sitting still for a few minutes.
A study in the Journal of the American Medical Association says to follow your RHR over time. “A healthy adult is expected to have RHR of 70,” says researcher Ulrik Wisloff, PhD. If your HRH increases more than 10 beats, says Wisloff, get a thorough check of your heart and blood vessels and ask your family doctor for advice about lifestyle changes.
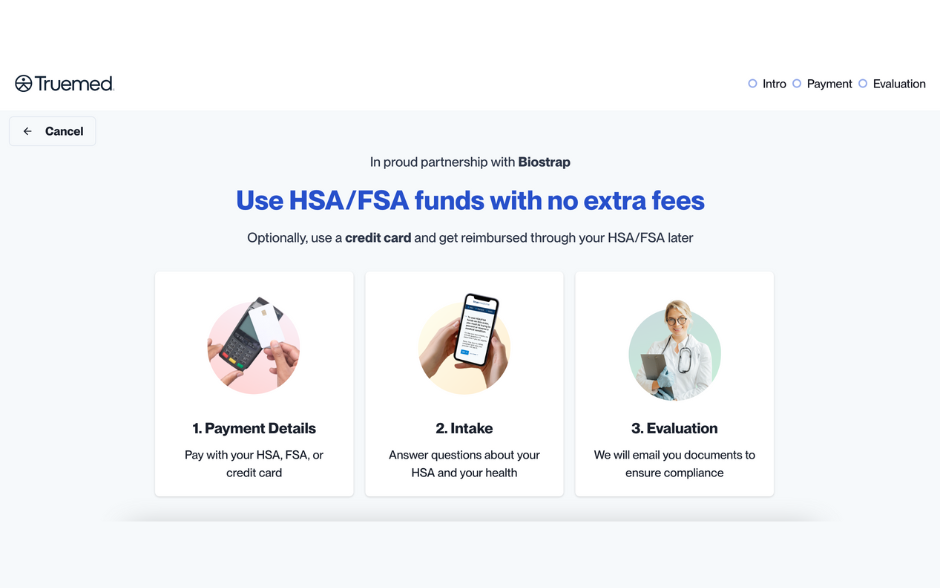
Digital health solutions, like Biostrap, now allow us to keep track of changes in our RHR. Given the research-driven paradigm shift, it’s not a moment too soon.