When it comes to getting enough sleep, we have a habit of trying to cut corners. Seven or eight hours of sleep may sound ideal, but rarely do we seem to have the time.
According to the National Sleep Foundation, older adults should sleep between 7-9 hours each night. This recommendation only increases amongst teenagers, preschoolers, and toddlers. Yet despite this advice, 45% of Americans say that poor or insufficient sleep has affected their daily lives at least once in the past week.
Getting a good night’s sleep isn’t easy, but it’s essential. Let’s pull down the sheets to learn more about sleep, why 6 hours of sleep simply isn’t enough for most people, and what we can do to ensure we’re getting the hours of shuteye we need.
The Basics of Sleep
There are four primary stages of sleep to be aware of, and we collectively refer to these stages as the sleep cycle.
The first stage is the lightest stage of sleep when you’re just dozing off. During this stage of drowsy sleep is when you may experience slight twitching such as Hypnic jerks, and you can also easily be woken. Your muscles will relax and your brain will begin to slow down as your body prepares for a more restful, deep sleep.
The second stage of sleep is when body temperature will begin to drop and heart rate and breathing rate both slightly decrease. You can’t be woken as easily during this stage of sleep, and your brain will continue to slow down as bursts of brain activity called sleep spindles occur. Research suggests sleep spindles protect the brain from awakening during sleep.
The third stage of sleep is known as slow-wave sleep. This is the most restorative stage of sleep and is marked by delta brain waves. Some of the most essential bodily processes occur during this stage including hormonal balancing, human growth hormone release, brain detoxification and memory consolidation.
The fourth and final stage of sleep is known as rapid eye movement, or REM, sleep, and this is where dreaming takes place. While your muscles will be “paralyzed”, brain waves will become more active, behaving nearly as if you were awake. Getting an adequate amount of REM sleep is very important for cognitive functions as well as memory.
Generally speaking, your body will spend more time in deep sleep during the first half of the night and more in REM during the second half.
Ensuring you reach each of these four stages of the sleep cycle is extremely important. One sleep cycle, which will include all four stages of sleep, will often last approximately 100-120 minutes, and you’ll transition through four or five full cycles per night.
For Most Of Us, 6 Hours of Sleep Isn’t Enough
We hate to burst your bubble, but six hours of sleep just isn’t enough for the average individual. While some people do well on only six hours of sleep, most of us would benefit from an extra hour or two of additional rest. Below we’ve included the nine primary sleep groups identified by the Centers for Disease Control and Prevention, along with their corresponding sleep recommendations.
Newborns
Newborns should receive between 14 and 17 hours of sleep, though 11 to 13 hours is acceptable as well. Ultimately, newborns shouldn’t sleep less than 11 hours per day.
Infants
Infants should sleep between 12 and 16 hours, including naps.
Toddlers
Toddlers should sleep between 11 and 14 hours each day, including naps. Toddlers shouldn’t sleep less than 9 hours per day.
Preschoolers
Preschoolers should sleep between 10 and 13 hours per day, including naps.
Children (6-12 years of age)
Children should get 9 to 12 hours of sleep.
Teens (13-18 years of age)
Teens should get 8 to 10 hours of sleep per day.
Adults (18-60 years of age)
Young adults should get 7 to 9 hours of sleep per day.
Older Adults (61-64 years of age)
Older should get 7 to 9 hours of sleep per day.
Seniors (65 years of age and older)
Seniors should get at least 7 to 8 hours of sleep each night.
Is 6 Hours of Sleep Enough for You?
While 6 hours of sleep isn’t enough for most of us, there are signs you can watch for to determine if 6 hours of sleep is enough for you. For instance, yawning, fatigue, brain fog, and irritability are telltale signs that you’re simply not getting enough sleep.
Other symptoms of tiredness or sleep loss include a lack of motivation, clumsiness, and increased appetite. If you’re sleeping for six hours or less per night while experiencing these symptoms, you’ll need to increase the amount of sleep you’re getting to reflect nightly recommendations for your age, or you’ll need to find ways to improve upon your quality of sleep.
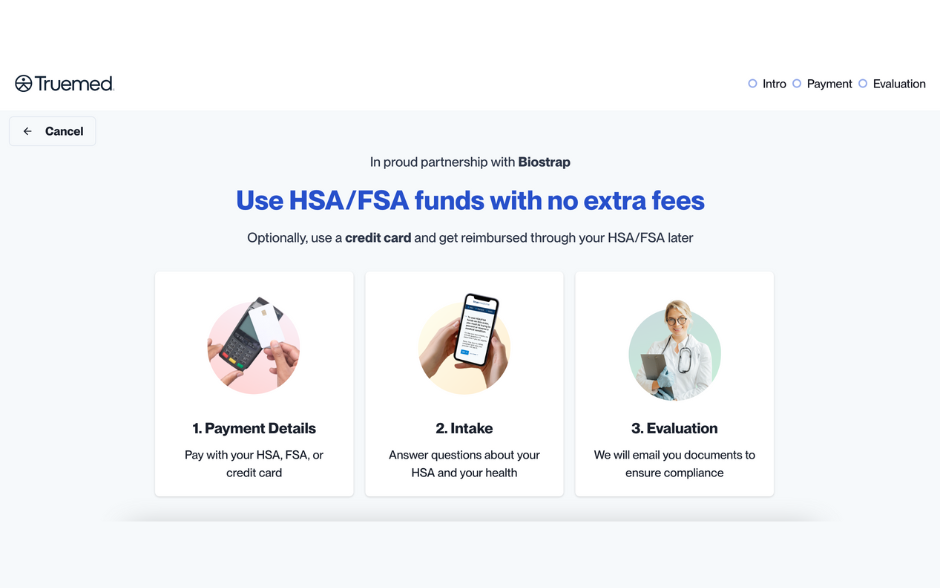
Did you know that Biostrap offers an advanced sleep tracking and analysis feature? In addition to the basic sleep offerings, the Biostrap Sleep Lab provides more frequent biometric recordings (up to every two minutes), plus after a 15-day baseline, you can get personalized sleep time and wake-up time recommendations to help optimize your circadian rhythm and achieve improved sleep quality and recovery.
Why Aren’t You Getting Enough Sleep?
Poor sleep or a lack of sleep can often be attributed to a number of factors. From taking sleep for granted to consuming caffeine before bed, sleep problems are widespread. Below you’ll find the common reasons people don’t get enough sleep.
Stimulants
Stimulants such as caffeine, alcohol, and even sleeping pills can interfere with your ability to fall asleep and stay asleep. While substances like alcohol may evoke the feeling of sleepiness, in reality, your sleep will be very restless. Sleeping medications, on the other hand, may be okay to use occasionally, but these become less impactful over time, and you may become dependent on them to fall asleep.
Shift Work
Those who work changing shifts have a more difficult time establishing a consistent sleep-wake pattern. While some adjust to these changes better than others, shift work can influence your circadian rhythm and drastically reduce the amount of sleep you should be getting each night.
Eating & Drinking Late
Eating late may impact the quality of your sleep. Going to bed on a full stomach will not only keep your body busy digesting what you just ate, instead of focusing on sleeping, but as elevated blood sugar levels trigger an insulin response, it can also cause a spike in cortisol which will keep you from transitioning into the sleep stages mentioned above.
Not to mention, certain unhealthy food choices may even cause heartburn, chest discomfort or bloating that may keep you up at night.
As a result, it’s best to avoid any late night snacks before bedtime. If you’re hungry, eat something small, such as a teaspoon of nut butter, and drink a glass of water or a cup of tea.
Stress
Stress may keep us up at night and disrupt our sleep schedule. Elevated stress levels may keep your fight-or-flight, or sympathetic nervous system, activated, blocking your chance to tap into the parasympathetic, rest-and-digest, nervous system and get a restful sleep. Give yourself a chance to relax and unwind before bed — meditate, journal or do some breathwork — to help your body wind down. If stress is still stopping you from getting quality sleep, speak with your doctor to find techniques for coping with stress.
Sleep Disorders
Sleep disorders are one of the most common reasons we suffer from sleep deprivation. Sleep apnea, night terrors, insomnia, and more can influence our sleep habits for days or even years at a time. If you suffer from a chronic sleep disorder that stops you from getting a good night’s sleep, consider talking to your doctor to determine what you can do to get back to bed.
Healthy Habits to Develop
Our body’s circadian rhythm is always telling us when it’s time to sleep and when it’s time to wake up. When this internal rhythm is disrupted, however, we’re left with a myriad of negative consequences leading to poor sleep. With this in mind, here are some tips on how to improve your sleep patterns so that falling asleep becomes a breeze.
Follow a Sleep Schedule
It may seem like a no-brainer, but your body prefers a sleep schedule that allows you to fall asleep and wake at the same time each day. This can also reduce your risk of heart disease, which sleep deprivation can increase your risk of developing.
Watch What You Eat
Avoid heavy meals close to bedtime and keep snacking to the minimum. Drinking water or tea before bed is healthy, but too much fluid can result in frequent bathroom trips that negatively impact your sleep duration.
Avoid Bedtime Distractions
Bedtime distractions such as digital screens, bright lights, and loud music can stop you from getting a good night’s sleep. Consider turning off your phone, dimming the lights, and reading a book before bed to allow your body and mind to wind down. A healthy bedtime routine that’s free of distractions will put your head in the right place before it hits the pillow.
Sleep Medicine
Though sleep medicine isn’t recommended for everyone, certain individuals may benefit from sleep medications that aid in falling asleep. If you find yourself suffering from a lack of sleep on a consistent basis, talk to your doctor to determine if sleep medicine is the right avenue for you.
So, Is Six Hours of Sleep Enough?
At the end of the day, six hours of sleep isn’t really enough for the average person. While we all know someone that functions well on less sleep, the side effects that come with a lack of sleep such as weight gain and compromised cognitive performance are reason enough to ensure you’re getting your recommended amount of sleep. While getting the sleep your body craves can be difficult, every hour of sleep you get makes an impact on your overall health.
Consider tracking your sleep with the most advanced digital health solution that’s available right now. Gain valuable insights into your sleep quality and start introducing a data-driven approach to understanding how your lifestyle choices are making an impact on your sleep and recovery.